T he foundation for each and every professional encounter begins with the case history; from a coding perspective, it is the most integral portion of your encounter. Since the adoption of the Resource Based Relative Value System (RBRVS), for coding compliance, the scorable elements of the case history were:
The chief complaint always drives the encounter, both from a perspective of what type of service you are providing—ophthalmic office visits or E/M visits—and the level of service provided. A properly recorded chief complaint also determines who is the responsible party for charges and payment for the respective services, whether it be a managed vision care plan, a medical carrier or the patient.
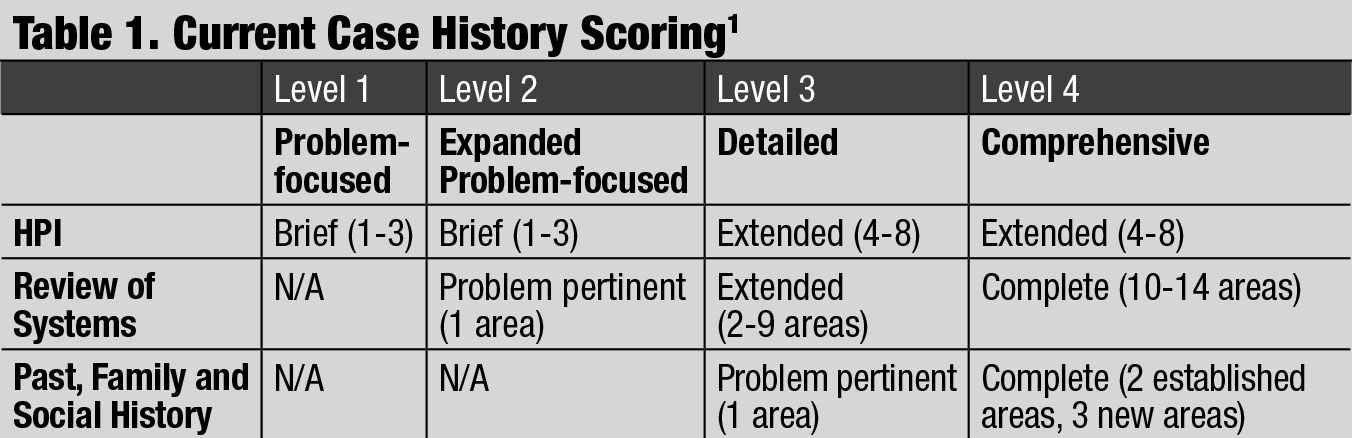 |
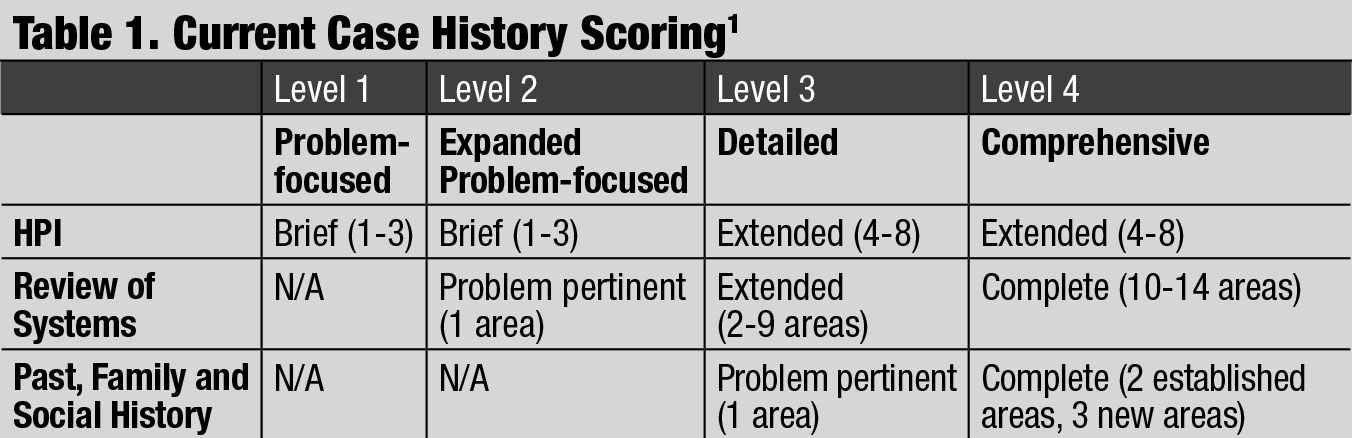
| Current Case History Scoring. Click table to enlarge. |
Four different levels of case history scoring exist: problem-focused, expanded problem-focused, detailed and comprehensive.
The case history is often overscored because individuals count all elements in the review of systems category that are asked and answered, rather than only those pertinent and germane to the chief complaint and patient presentation.
From a rules perspective, traditionally, the physician had to retake and reenter all of the information about the patient’s chief complaint and history that a staff member had already taken; but as of 2019, physicians only have to document in the medical record that they “reviewed and verified” the chief complaint and history information already recorded by ancillary staff or the patient, thus saving time and eliminating redundancy for all.
In our current system, the level case history you perform must be commensurate with the patient’s presenting problem. You cannot perform the same level of case history on everyone because it is “your standard of care.” It must be an individualized case history based upon the patient’s presenting problem.
Beginning January 1, 2021, the case history will no longer be individually scored as it contributes to the level of E/M service performed. The history and physical will not be elements for code selection and scoring. While capturing the patient’s pertinent history and performing a relevant physical exam contributes to the physician’s time and medical decision making, these elements alone should not determine the appropriate code level. The AMA and CMS workgroup revised the code descriptors to state that providers should perform a “medically appropriate history and/or examination,” so next year the individual elements of the history taken won’t matter with respect to the level of office visit.
To illustrate, the 2021 definition of a 99203 eliminates specific language about component requirements and leaves things more in the physician’s hands. The current definition states: office or other outpatient visit for the evaluation and management of a new patient, which requires these three components: a detailed history; a detailed examination; medical decision making of low complexity. Counseling and/or coordination of care with other providers or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the presenting problem(s) are of moderate severity. Physicians typically spend 30 minutes face-to-face with the patient and/or family.
The 2021 definition is: office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and low level of medical decision making. When using time for code selection, 30 to 44 minutes of total time is spent on the date of the encounter.
Case history will always remain the foundation for type and level of services performed and a key element to determine the scoring of your professional services. Changes in 2019 and those coming in 2021 will give you more control of what you do and how you do it, while still being compliant with CPT guidelines and rules.
Send your coding questions to rocodingconnection@gmail.com.
| 1. Department of Health and Human Services. Evaluation and management services. www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/eval-mgmt-serv-guide-ICN006764.pdf. Accessed December 30, 2019. |